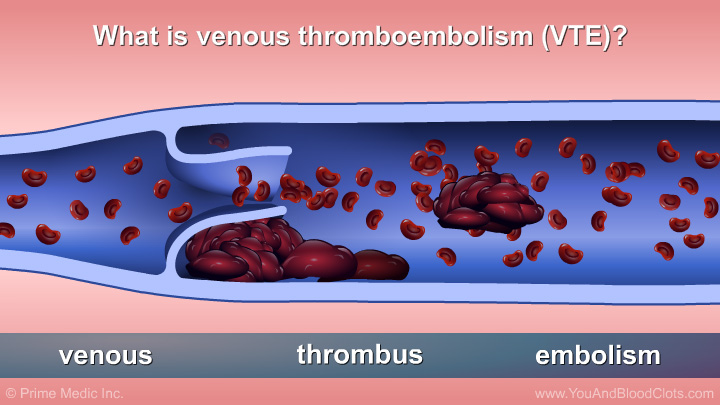
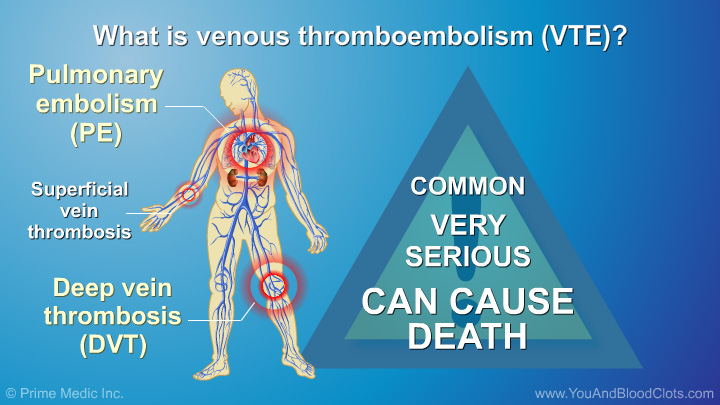
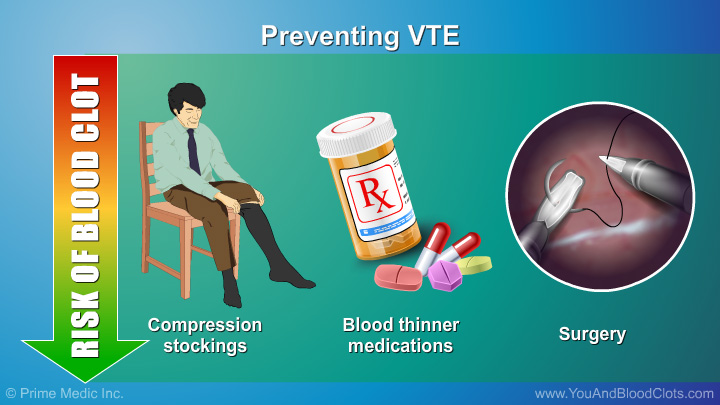

Watch this slide show to learn about the medications and treatments most commonly used for venous thromboembolism (VTE), as well as how they work and how they are taken. The main types of treatments are anticoagulants (also called blood thinners) and thrombolytic therapy (also called clot busters). The use of compression stockings and vena cava filters are also explained.
This animation explains the medications and treatments most commonly used for venous thromboembolism (VTE), as well as how they work and how they are taken. The main types of treatments are anticoagulants (also called blood thinners) and thrombolytic therapy (also called clot busters). The use of compression stockings and vena cava filters are also explained.
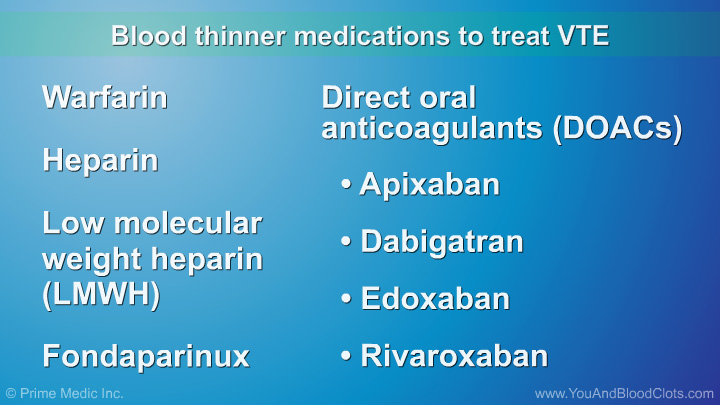
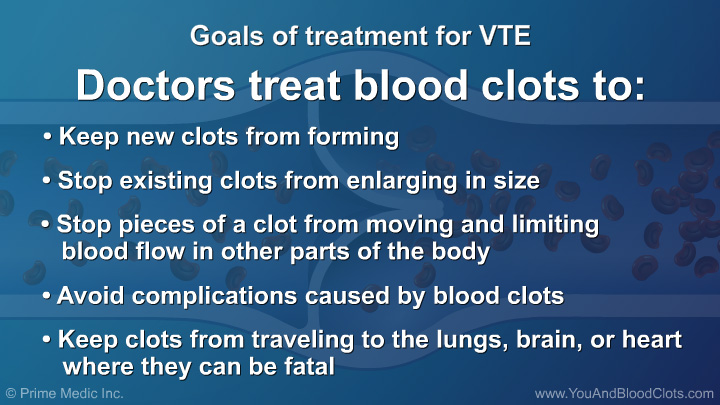
Anticoagulants (also referred to as “blood thinners”) are the medications most commonly used to treat venous thromboembolism (VTE) blood clots. In this video Dr Sandra Adams explains that blood thinners make it harder for blood to clot, lower the chances of patients forming new clots, reduce the risk of existing clots growing bigger, and allow the body to dissolve the clot over time. Blood thinners include heparin, low molecular weight heparin, warfarin, fondaparinux, apixaban, dabigatran, edoxaban, and rivaroxaban. On rare occasions, other medications may be needed.
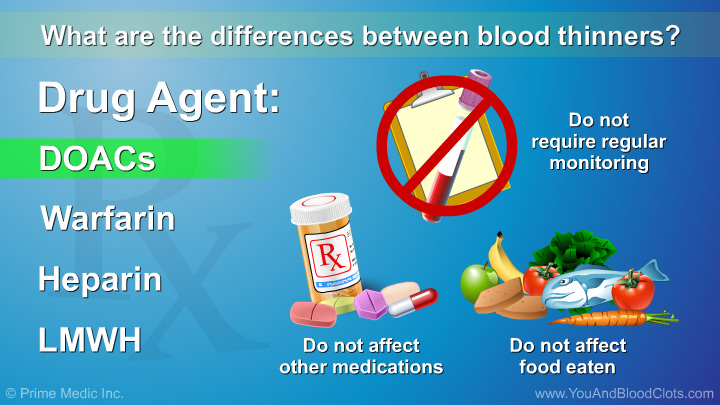
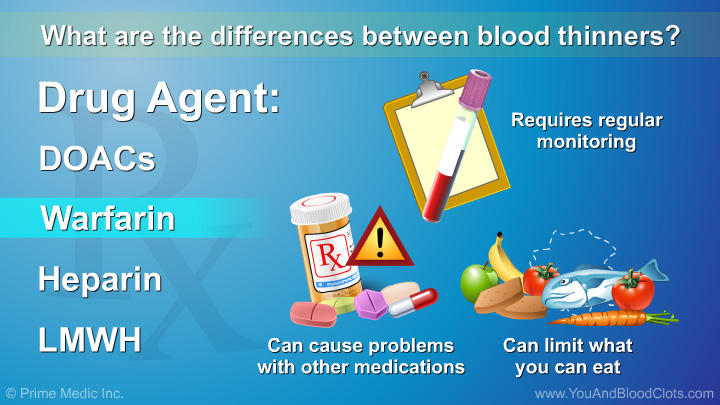
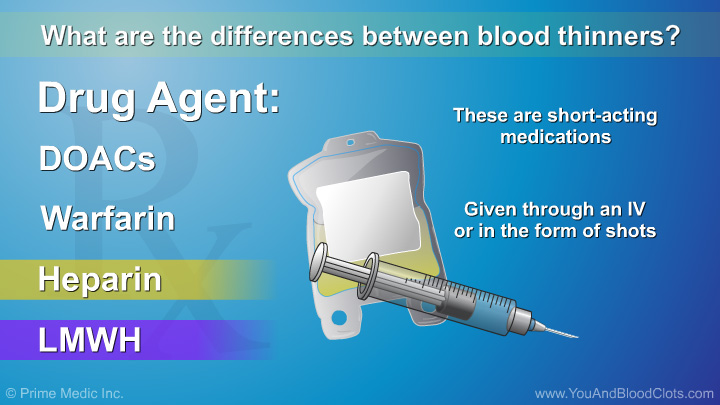
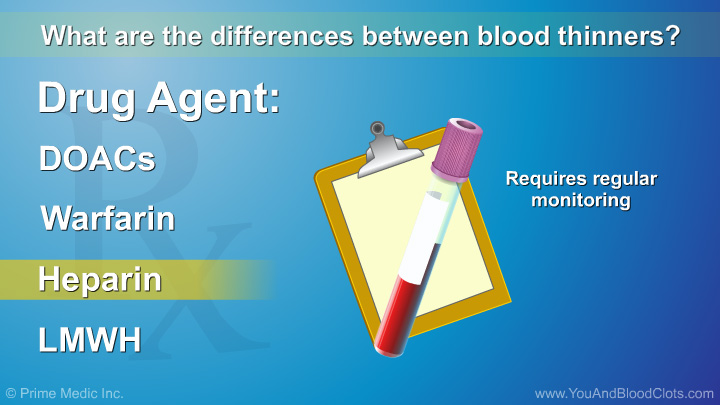
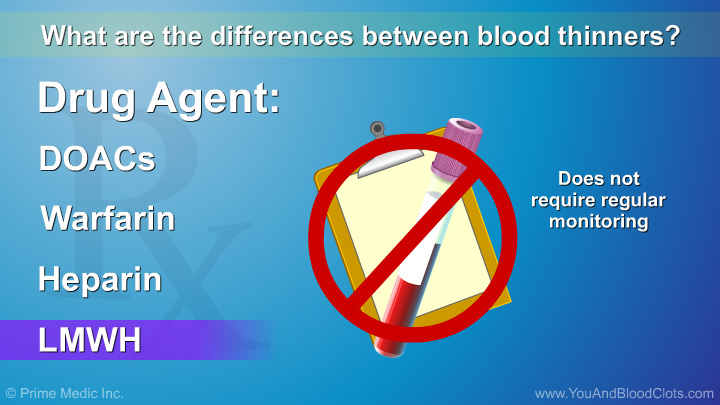
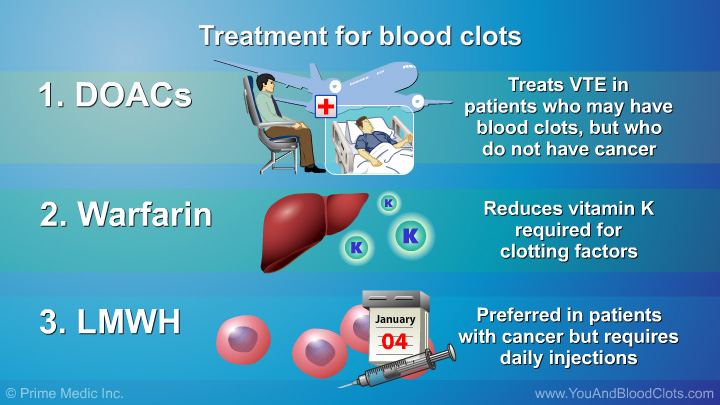
In this video, Dr Sandra Adams explains how older and newer blood thinners work for the treatment of VTE blood clots, and how they are taken. The main older blood thinner used is called warfarin, which blocks the liver from making the clotting proteins that require vitamin K. If you are taking Warfarin you will need frequent monitoring with blood tests. Warfarin is also affected by other medications and your diet because high levels of Vitamin K are found in dark green or leafy vegetables. The newer blood thinners fall into two groups. The first group includes low molecular weight heparin and fondaparinux that are taken as shots. These medications are much more predictable than warfarin and do not require frequent monitoring with blood tests. The second group includes pills that are taken by mouth, such as apixaban, dabigatran, edoxaban, and rivaroxaban. They do not require monitoring, are not affected by other medications or food, and work very quickly. All of these medications have been shown to work well to prevent more blood clots from forming.
Dr Sandra Adams explains in this video that a number of factors go into deciding what is the best blood thinner for each patient with VTE blood clots, including: how well your kidneys work, if you have any liver damage, your weight, what you usually eat, any other illnesses you may have, and how often you can see a healthcare professional for follow up visits and monitoring. Your physician will evaluate your current condition and your medical history to recommend a blood thinner that best suits you.
Blood thinners are lifesaving medications because they can treat or prevent VTE blood clots. The biggest safety concern for anyone taking a blood thinner is the risk of bleeding, explains Dr Sandra Adams in this video. This risk of bleeding may be slightly lower with the newer agents than for warfarin. If you are taking blood thinners, you should be very careful to avoid hurting yourself. Because blood thinners prevent clotting, a tiny cut or bruise will bleed a lot more if you are taking blood thinners. Even if you don't have a cut or bruise, a bump or fall could cause you to bleed internally. Therefore, when taking blood thinners, your body may need help to stop the bleeding. Be sure to discuss the benefits and risks of blood thinners with your health care professional.
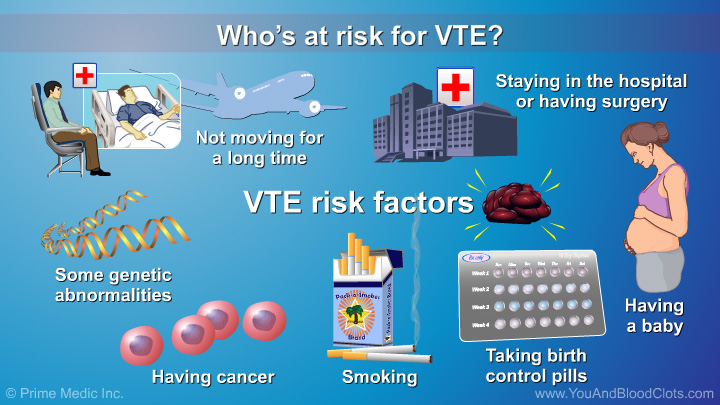
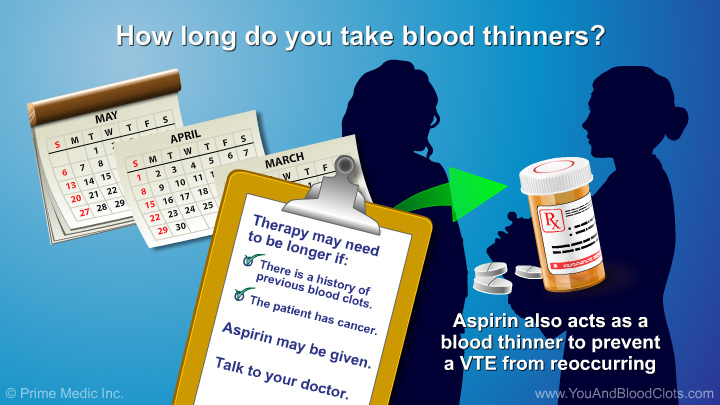
Dr Sandra Adams explains in this video that if you are taking blood thinners you should have regular follow up visits with your doctor to make sure your medications are working well and that there are no serious side effects. If you are on warfarin, you will need to go in for more frequent check-ups to make sure that you are getting enough to reduce the risk of blood clots, but not so much that you have a high risk of bleeding. Most patients take blood thinners for at least 3 months, but the length of time will vary based on your personal risk factors. People with cancer need to be treated until the cancer is gone. People who have had blood clots before may need to take blood thinners for the rest of their lives.
In this video, Dr Sandra Adams explains that warfarin is in the same family as some of the older chemicals that were used to kill rats, but it is not rat poison. Warfarin has been used in humans with good results for many years. It is still a very effective and safe medication when used correctly and monitored closely. Any blood thinner can cause bleeding and should be monitored closely. Be sure to discuss the benefits and risks of blood thinners with your health care professional.
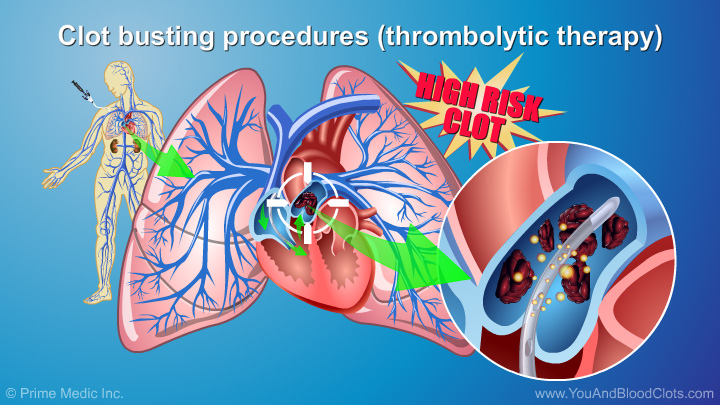
The most commonly used medications to treat VTE blood clots are anticoagulants (also referred to as “blood thinners”). But there are also “clot busting” medications called thrombolytics which quickly dissolve or get rid of clots. As Dr Sandra Adams explains in this video, thrombolytic therapy may be used depending on the resources available at your hospital and your doctor’s opinion of how likely your clot will cause harm in the long run. Clot buster medications increase the risk for major bleeding so they are usually reserved for patients with very extensive clots and for life-threatening situations.
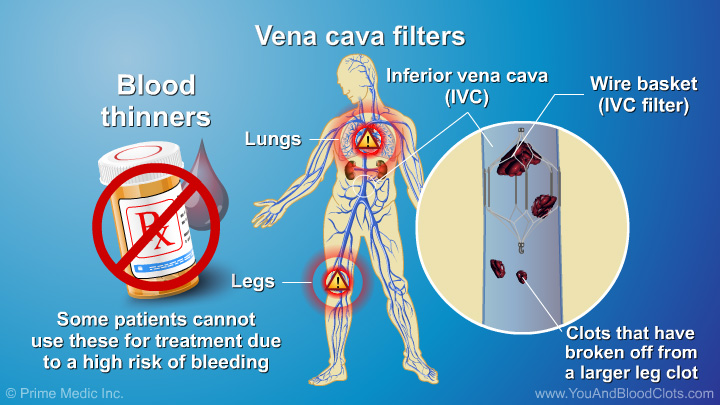
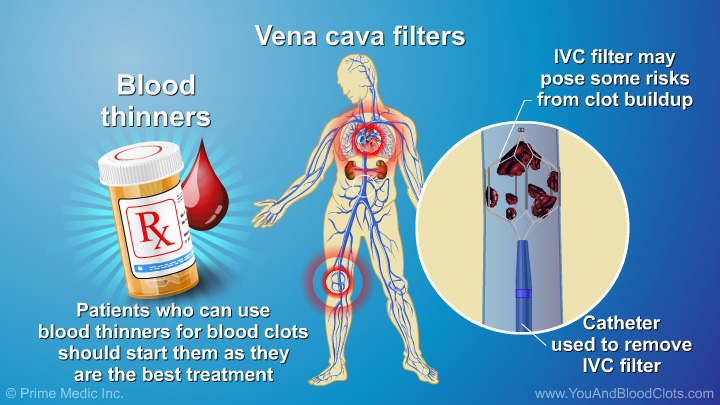
Most patients will recover from their blood clot after it is recognized and treated, but as Dr Sandra Adams explains, sometimes surgery is needed for patients with high-risk blood clots. In a small number of patients whose bodies are not able to completely dissolve their blood clots, surgery may be needed to remove the scars caused by the blood clots. Other patients cannot be treated with blood thinners due to a high risk of bleeding or because they started to bleed on a blood thinner. If a patient with VTE blood clots cannot take blood thinners, a wire basket or filter may be placed in the large vein (or vena cava) to catch any clots that might break off from the leg veins and go to the lungs.
Jointly provided by Postgraduate Institute for Medicine, WipeDiseases Foundation and Prime Medic Inc.
This activity is supported by an independent educational grant from Daiichi Sankyo.
This website is part of the Animated Patient™ series developed by Prime Medic Inc., to provide highly visual formats of learning for patients to improve their understanding, make informed decisions, and partner with their healthcare professionals for optimal outcomes.